This report originally appeared on nih.gov. To view the full report, click here.
The HHS Panel on Antiretroviral Guidelines for Adults and Adolescents (the Panel) has just released an updated version of the Guidelines for the Use of Antiretroviral Agents in Adults and Adolescents with HIV.
Key updates in this version of the guidelines include:
- Antiretroviral Therapy to Prevent Sexual Transmission of HIV: Clinical trials have shown that using effective antiretroviral therapy (ART) to consistently suppress plasma HIV RNA levels to <200 copies/mL prevents transmission of HIV to sexual partners. When ART is used to prevent HIV transmission, this strategy is called treatment as prevention (TasP). The Panel has added a new section to the guidelines to help providers integrate TasP into their clinical practice.
- The latest data on neural tube defects (NTDs) in infants born to women who received dolutegravir (DTG) around the time of conception have shown that the prevalence of NTDs is lower in these infants than initially reported. Based on the new data, the Panel has revised some recommendations related to the use of DTG in individuals who are of childbearing potential and who are trying to conceive, those who are sexually active and not using contraception, and those who are using effective contraception.
- What to Start: The Panel has added DTG plus lamivudine to the list of Recommended Initial Regimens for Most People with HIV, except for individuals who have pre-treatment HIV RNA >500,000 copies/mL, who are known to have active hepatitis B virus (HBV) coinfection, or who will initiate ART before results of HIV genotype testing for reverse transcriptase or HBV testing are available.
- Cost Considerations and Antiretroviral Therapy: A new sub-section on cost sharing that describes how varying cost-containment practices may impact the out-of-pocket payments for patients with Medicaid, Medicare, and Ryan White (AIDS Drug Assistance Program) coverage has been added. To help clinicians better understand the different ART-related pricing systems in the United States, a new table titled Table 19a. Insurance and Health Program Prescription Drug Pricing and Access was created.
- Acute and Recent (Early) HIV Infection: Bictegravir/tenofovir alafenamide/emtricitabine has been added as a treatment option for persons with acute or recent HIV infection in cases where ART will be initiated before genotypic drug resistance testing results are available.
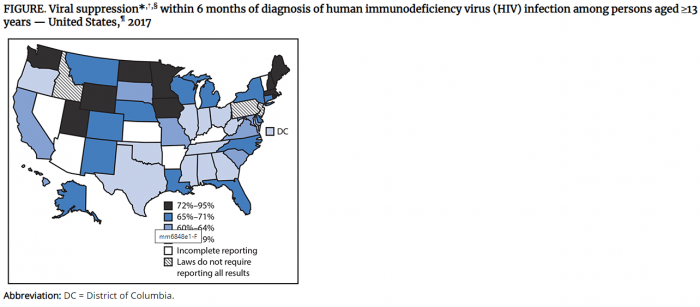
- Initiation of Antiretroviral Therapy: The Panel recommends that ART be started immediately or as soon as possible after diagnosis to increase the uptake of ART, decrease the time required to achieve linkage to care and virologic suppression for individual patients, reduce the risk of HIV transmission, and improve the rate of virologic suppression among persons with HIV.
- Laboratory Testing for Initial Assessment and Monitoring of People with HIV Receiving Antiretroviral Therapy: The Panel previously recommended monitoring fasting lipid profile and fasting glucose before and after initiating ART. This section now includes a new recommendation that allows for random (nonfasting) tests.
- Tuberculosis/HIV Coinfection: This section now includes newly published data on short-course regimens in the treatment of latent tuberculosis infection and new drug-drug interaction data for antiretroviral drugs and rifampin and rifapentine.
For a complete list of guideline updates, please see What’s New in the Guidelines. Additions and revisions are also highlighted in yellow throughout the PDF version of the guidelines.
To view or download the guidelines, go to the Adult and Adolescent Antiretroviral Guidelines section of AIDSinfo’s website. The guideline tables and the boxed recommendations can also be downloaded as separate PDF files.





 Research Laboratories, MRL 1-441. Dr. Sibeko’s work has focused on interventions using non-specialist workers in the management of severe mental illness, and he has a developing research portfolio focused on task sharing models for the treatment of harmful substance use, mental health and HIV.
Research Laboratories, MRL 1-441. Dr. Sibeko’s work has focused on interventions using non-specialist workers in the management of severe mental illness, and he has a developing research portfolio focused on task sharing models for the treatment of harmful substance use, mental health and HIV.