This post originally appeared on the NIAID NIH website. To see the original article, click here.
Today marks not just a time to exchange valentines and chocolates, but also the midpoint of American Heart Month. Did you know people living with HIV are at an increased risk of experiencing cardiovascular disease? Fortunately, NIH-supported research is getting to the heart of the problem.
 Effective anti-HIV medications dramatically reduced the number of AIDS-related deaths in the United States. However, because people with HIV are now able to live longer than before, cardiovascular disease has emerged as a leading cause of death among people living with HIV. In fact, studies have shown that a person living with HIV is up to twice as likely as someone who does not have HIV to experience a heart attack or stroke—even when the virus is well controlled with antiretroviral therapy.
Effective anti-HIV medications dramatically reduced the number of AIDS-related deaths in the United States. However, because people with HIV are now able to live longer than before, cardiovascular disease has emerged as a leading cause of death among people living with HIV. In fact, studies have shown that a person living with HIV is up to twice as likely as someone who does not have HIV to experience a heart attack or stroke—even when the virus is well controlled with antiretroviral therapy.
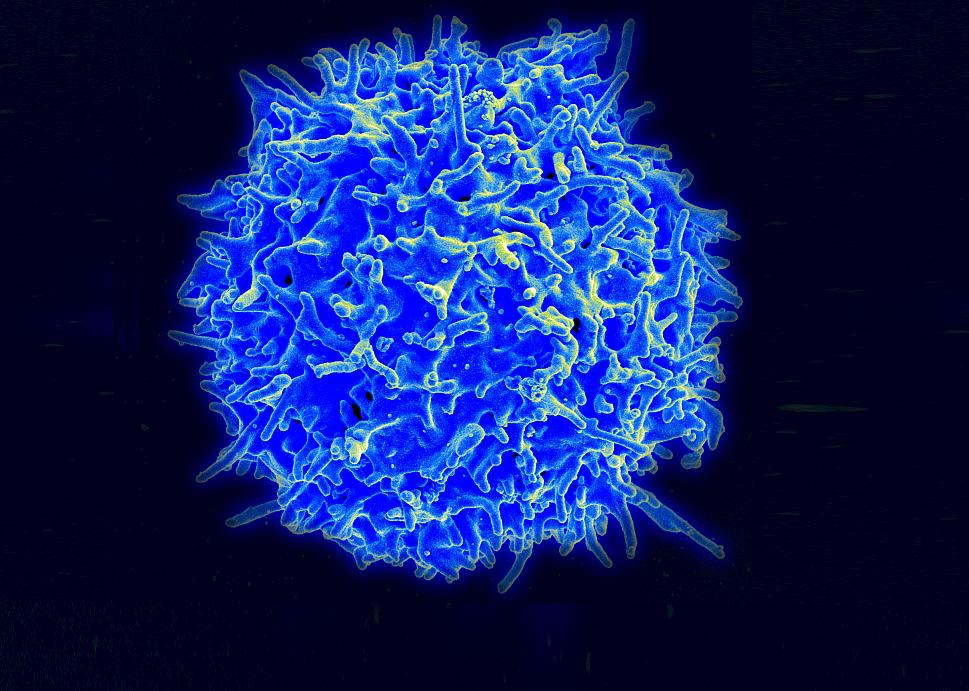
How can a disease of the immune system affect the heart? Scientists at the NIH and elsewhere have observed that HIV infection, even in people with HIV whose infection is well-controlled with antiretroviral therapy, leads to persistent immune system activity in a person’s body. This chronic activation can lead to both a surplus of clotting compounds and inflamed blood vessels. Left unchecked, these factors increase an individual’s risk of a life-threatening heart attack or stroke.
This effect can be exacerbated by traditional risk factors for heart disease, such as smoking, an unhealthy diet, inactivity and a family history of cardiovascular problems. So, it is especially important for people living with HIV to eat well, stay active, avoid tobacco and know their family health history.
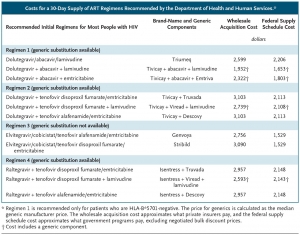
To see if the risk can be decreased further, NIAID and the National Heart, Lung and Blood Institute, both parts of NIH, launched the Randomized Trial to Prevent Vascular Events in HIV, or REPRIEVE, in April 2015. The study plans to enroll at least 6,500 participants between the ages of 40 and 75 to determine if a daily dose of a cholesterol-lowering statin can reduce the risk of heart disease in people living with HIV who would not normally be prescribed a statin based on traditional methods of estimating cardiovascular disease risk.
The first large clinical trial to do so, REPRIEVE is investigating a strategy to prevent HIV-related heart disease in the United States and internationally. By collecting data from volunteers throughout the world, REPRIEVE seeks to expand our knowledge of how HIV and heart disease are related, and how men and women living with HIV can continue to live well into their 60s, 70s and beyond.
Learn more about the REPRIEVE trial: