A Message from CHIPTS:
On this World AIDS Day, we stand in solidarity with all those living with, at risk for, or affected by HIV across the world. It is both a sobering and an exciting time.
We are currently faced with a challenge and an opportunity for bending the arc of new HIV infections toward zero in the United States. The U.S. Government has identified “Ending the HIV Epidemic” as a top issue for the administration – promising resource support necessary to end the domestic HIV epidemic. This is a clarion call for cooperation and synergy between public health professionals, clinicians, scientists and communities. Bold initiatives are required. Now is the time.
Implementing wider reaching, better and faster HIV treatment and prevention will uncover known and unknown challenges to the goal of eliminating HIV. We know the current models of treatment and prevention, organized around getting medications into the hands of those who need them – especially people living with HIV – has helped improve health and reduce new transmissions. Pre-exposure prophylaxis, antiretroviral medications used to support remaining HIV-negative, has potential for further reducing new infections.
Disparities in access to care, medical mistrust, racism, sexism, homophobia, transphobia, and HIV-associated stigma are all contributing to unequal benefits of the cornucopia of tools we currently possess to both treat those affected by, and at-risk for HIV. We must address these as an overarching priority or we will fail: we will fail ourselves, our colleagues, our patients, our clients, our constituents, and the epidemic writ large.
The potential for an infusion of new resources into ending the HIV epidemic is therefore both exciting and daunting. We must fight in an environment in which health systems increasingly seem at cross-purposes or even antithetical to these goals and visions.
We must recognize and address that a sizeable minority, perhaps 15%-20% of people living with HIV or with high risks for HIV infection, need more, better, and/or different interventions – now and into the foreseeable future – to ensure consistent adherence with HIV care and persistence with HIV prevention. This part of the strategy recognizes that for many in this minority, chronic and relapsing conditions often interfere with efforts to sustain consistent medication taking, whether for HIV care or HIV prevention. These conditions include mental health and/or substance use disorders, in addition to the “isms” listed above.
We need partnerships and regional responses. We must recognize the impacts of gentrification and other social and economic factors displace large numbers of Americans from affordable housing, which challenges implementation of new resources in HIV-care and prevention so that they reach the people who need them.
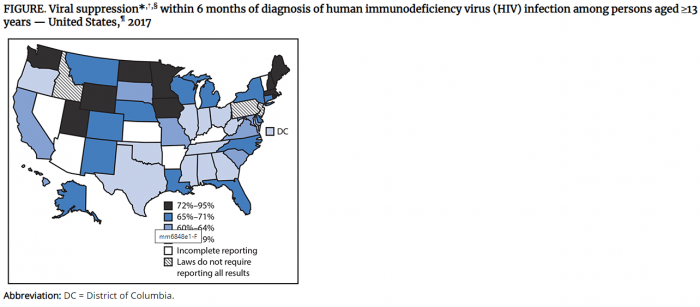
We need better, faster, more flexible ways to measure HIV outcomes and current factors that correlate with outcomes from investments across regions. Health jurisdictions are not configured to measure regional outcomes.
Making measurable progress in ending the HIV epidemic in the U.S. is a thrilling possibility. And to reach this objective carries the real possibility that we will learn that improving health outcomes for the most of us are directly tied to ensuring that we improve the health outcomes for all of us. But only if all involved work together, with redoubled and common resolve, to end these inequities, address the clearly identified social determinants of health, in partnership and on equal footing with more conventional advances in biomedical science.
Here’s to thinking out of the box on this World AIDS Day.