This article originally appeared on hptn.org. To see the full article, click here.
DURHAM, N.C. – Researchers from the HIV Prevention Trials Network (HPTN) announced today that the HPTN 083 clinical trial showed that a pre-exposure prophylaxis (PrEP) regimen containing long-acting cabotegravir (CAB LA) injected once every 8 weeks was superior to daily oral tenofovir/emtricitabine (TDF/FTC) for HIV prevention among cisgender men and transgender women who have sex with men. The results were reported at the 23rd International AIDS Conference (AIDS 2020: Virtual). HPTN 083 is a randomized, controlled, double-blind study comparing the safety and efficacy of a regimen including CAB LA to daily TDF/FTC at 43 sites around the world.
An independent Data and Safety Monitoring Board (DSMB) that reviewed interim study data in May 2020 found that the PrEP regimen including CAB LA injected once every 8 weeks safely and effectively prevented HIV acquisition in the study population. Consequently, the DSMB recommended stopping the blinded comparison, offering CAB to all study participants, and disseminating the results. The final analysis of these data demonstrates the superiority of CAB compared to TDF/FTC for PrEP in the HPTN 083 study population.
“The HPTN 083 results demonstrating the superiority of CAB to TDF/FTC have the potential to transform the landscape of HIV prevention for cisgender MSM and transgender women,” said HPTN 083 protocol chair Dr. Raphael J. Landovitz. “We know that some people have difficulty with or prefer not to take pills, and an injectable product such as long-acting CAB could be a very important option for them. We want to thank the study participants and research staff, as this study would not have been possible without their dedication and commitment.” Dr. Landovitz is a professor of medicine at the David Geffen School of Medicine at the University of California, Los Angeles (UCLA) and co-director of the UCLA Center for Clinical AIDS Research & Education (CARE).
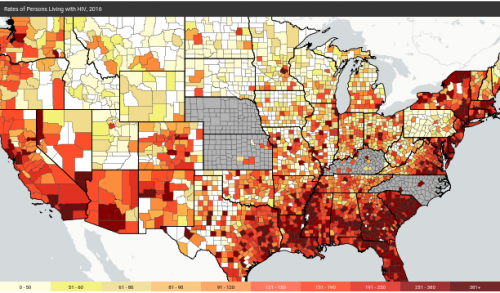
Overall, HPTN 083 enrolled 4,570 cisgender men and transgender women who have sex with men at research sites in Argentina, Brazil, Peru, South Africa, Thailand, the U.S., and Vietnam. Two-thirds of study participants were under 30 years of age, and 12% were transgender women. Half of the participants in the United States identified as Black or African American.
Read more about the HPTN 083 Study findings.
For general information about the HPTN 083 Study, visit the HPTN 083 website.
Dr. Raphael Landovitz, Co-Director of CHIPTS and the CHIPTS Combination Prevention Core, presented study findings on behalf of the HPTN 083 Team at this year’s AIDS 2020 conference. A copy of this slide presentation is also available on the HPTN 083 website here.