October 15 – Today, CHIPTS commemorates National Latinx AIDS Awareness Day (NLAAD), a day dedicated to recognizing the impact of HIV in the Latinx community. In honor of NLAAD, CHIPTS Combination Prevention Core Scientist Dr. Ronald A. Brooks shares a reflection on the impact of HIV among Latinx persons and recommended approaches to end the HIV epidemic in the Latinx community.
Dr. Brooks has dedicated his entire career here at UCLA to social-behavioral HIV research with Latinx sexual and gender minority populations. He also currently serves as the Interim Director of Research and Evaluation at Bienestar Human Services, one of the largest Latinx HIV service organization in the U.S. Read Dr. Brooks’ reflection below.
National Latinx AIDS Awareness Day

Each year on October 15th we observe National Latinx AIDS Awareness Day (NLAAD) to bring attention to the impact of HIV on Latinx persons in the United States. NLAAD is a day to re-invigorate our commitment to promoting HIV awareness and testing, disseminating effective HIV prevention strategies such as pre-exposure prophylaxis (PrEP), linking people to care for improved health outcomes, and working toward reducing HIV disparities and creating greater health equity in the Latinx community.
According to the CDC, Latinx persons accounted for over a quarter (28%) of all new HIV infections in the U.S in 2019, at a rate that was three times higher than that among non-Hispanic White persons. The overwhelming majority of new HIV infections in the Latinx community were among gay and bisexual men and other men who have sex with men. Another group severely impacted by HIV are Latina transgender women. The CDC’s recent HIV Surveillance Special Report assessing HIV Infection, Risk, Prevention, and Testing Behaviors Among Transgender Women in 7 US Cities, 2019-2020 found that 35% of Latina transgender women had HIV. For many Latinx sexual and gender minority persons, HIV looms like an omnipresent dark cloud over their lives. Moreover, one in six Latinx persons in the U.S. is unaware of their HIV status. As a result, they cannot take advantage of early HIV treatment to improve their health outcomes, and may continue to transmit HIV to others. With new HIV infections continuing to impact Latinx persons, now, more than ever, is the time to act to bring an end to the HIV epidemic in this community.
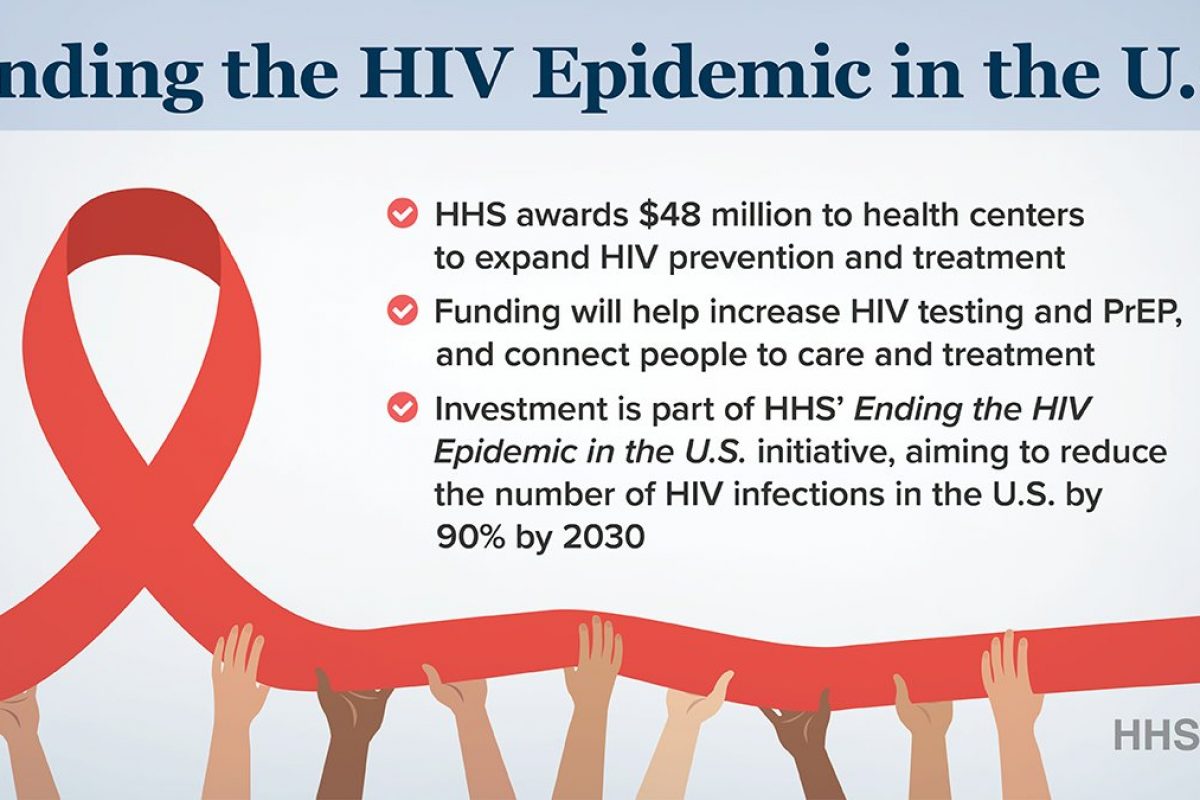
We have the tools to bring an end to the HIV epidemic among Latinx persons. Today’s HIV medications are simpler to take and less toxic and can help persons achieve viral suppression so they can no longer transmit the virus to others. PrEP is highly effective biomedical prevention strategy that can help reduce the rate of new HIV infections. However, multiple systemic, community, and individual-level barriers hinder access to these tools among Latinx persons. Barriers include experiences of stigma and discrimination resulting from homophobia, transphobia, and racism, and intersectional stigma stemming from the multiple marginalized identities of many Latinx persons (e.g., immigration status and lack of documentation, monolingual Spanish speaking, substance use disorder, sexual orientation, gender identity). Other systemic barriers include poverty and lack of access to quality health care services. On NLAAD, it is important to think about what interventions and resources are needed by Latinx communities across the country to help overcome these barriers and bring an end to HIV among all Latinx persons. In addition, it is important to consider the role that trusted Latinx community-based organizations can play in providing these HIV services to the community in a culturally affirming and respectful manner.
Moving forward, addressing the HIV epidemic among Latinx populations will require shifting our approach to be “status neutral.” This approach integrates prevention and treatment services so that both become part of the fabric of comprehensive primary prevention and care. By no longer separating these areas of HIV into silos, we can help mitigate HIV-related stigma that continues to plague our prevention and treatment efforts with this population.
Today, on NLAAD, I am encouraged by a new wave of emerging Latinx community leaders working in HIV prevention and treatment. These leaders are forging new and stronger partnerships with academic HIV researchers and public health departments to take on the HIV battle in novel and innovative ways. These partnerships involve more inclusion and participation of community in HIV research with Latinx populations — partnerships that will result in the creation of culturally-centered and more impactful strategies and interventions to end the HIV epidemic affecting all Latinx populations.





 The resources for women aim to educate them about the benefits of PrEP, to encourage them to seek more information, and to engage in discussions with their health care providers to determine if PrEP is right for them. Implementation includes both organic and paid social media efforts, and ads on dating apps, digital web banners, digital radio, and video streams.
The resources for women aim to educate them about the benefits of PrEP, to encourage them to seek more information, and to engage in discussions with their health care providers to determine if PrEP is right for them. Implementation includes both organic and paid social media efforts, and ads on dating apps, digital web banners, digital radio, and video streams.
