WASHINGTON: Researchers have decoded a system that renders certain types of immune cells impervious to HIV infection, paving way for its possible eradication from the body.
WASHINGTON: Researchers have decoded a system that renders certain types of immune cells impervious to HIV infection, paving way for its possible eradication from the body.
The researchers say the discovery points toward a new approach to eradicating HIV from the body, the journal Proceedings of the National Academy of Sciencesreported.
“For decades, we’ve seen conflicting reports on whether each of these components helped protect cells from viruses,” said James Stivers, from the Johns HopkinsUniversity.
“By plotting how much of each are found in different types of cells, as well as the cells’ response to HIV, we learned that both are needed to get the protective effect,” Stivers said in a statement.
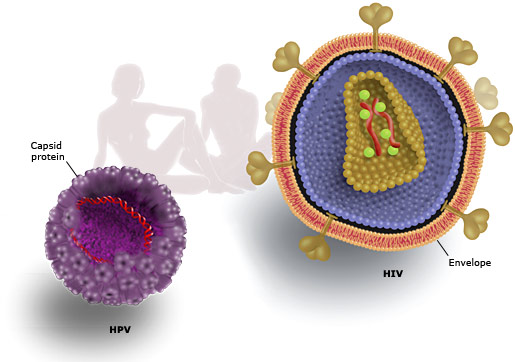
DNA’s code is made up of four building blocks called nucleotides, commonly abbreviated A, T, G, and C.
Before a cell divides, DNA-copying enzymes string these nucleotides together based on existing templates, so that each of the new cells gets its own copy of the genome.
Because the T nucleotide, dTTP, is very similar to dUTP, a fifth nucleotide that doesn’t belong in DNA, the copying enzyme sometimes mistakenly puts in a U instead of a T.
To prevent this, Stivers says, most human cell types have an enzyme whose job is to break down dUTP, keeping its levels very low. Another quality control measure is the enzyme hUNG2, which snips stray Us out of newly copied DNA strands, leaving the resulting holes to be filled by a different repair enzyme.
Certain immune cells called resting cells lack the first quality-control mechanism because “they’re not replicating their DNA and dividing, so they couldn’t care less if they have a lot of dUTP”.
Stivers says, when a retrovirus like HIV invades a cell, its first order of business is to make a DNA copy of its own genome, then insert that copy into the host cell’s genome.
If there are many dUTPs floating around in the cell, they will likely make their way into the new viral DNA, and, potentially, later be snipped out by hUNG2.
Researcher Amy Weil measured dUTP levels and hUNG2 activity in a variety of human cells grown in the laboratory, then exposed them to HIV.
Cells with high dUTP but little hUNG2 activity succumbed easily to the virus, which appeared to function just fine with a U-ridden genome.
Similarly, cells with low dUTP levels but high hUNG2 activity were susceptible to HIV. For these cells, it seemed, hUNG2 would snip out the few stray Us, but the resulting holes would be repaired, leaving the viral DNA as good as new.
But in cells with both high dUTP and vigilant hUNG2, the repair process turned into a hack job, Stivers says, leaving the viral DNA so riddled with holes that it was beyond repair.
Stivers says, the study identifies a new pathway that could restrict HIV infection in non-dividing cells.
From The Economic Times





 WASHINGTON: Researchers have decoded a system that renders certain types of immune cells impervious to
WASHINGTON: Researchers have decoded a system that renders certain types of immune cells impervious to