|
“HIV decreases BDNF in WIHS women……BDNF is critical for neuronal survival……recent data have shown a relationship between BDNF in blood and Alzheimer’s disease [20] and age-related cognitive impairment…….The research team found that even though HIV does not infect neurons, it tries to stop the brain from producing a protein growth factor – mature brain derived neurotrophic factor (mature BDNF)……acts like “food” for brain neurons. Reduced mature BDNF results in the shortening of the axons and their branches that neurons use to connect to each other, and when they lose this communication, the neurons die…….serum BDNF could be a predictor of risk for the development of neurological signs in HIV-positive individuals. Our findings…….provide initial evidence in support of this hypothesis and suggest this neurotrophin (BDNF) as a possible biomarker for HIV dementia…..Mocchetti believes that HIV stops production of mature BDNF because that protein interferes with the ability of the virus to attack other brain cells. It does this through the potent gp120 envelope protein that sticks out from the viral shell – the same protein that hooks on to brain macrophages and microglial cells to infect them. “In earlier experiments, when we dumped gp120 into neuronal tissue culture, there was a 30-40 percent loss of neurons overnight. That makes gp120 a remarkable neurotoxin.””
“The findings suggest a possible therapeutic intervention…….to use a small molecule to block the p75NTR receptor that proBDNF uses to kill neurons. A small molecule like that could get through the blood-brain barrier…….”If this works in HIV-dementia, it may also work in other brain issues caused by proBDNF, such as aging”
How HIV Affects the Brain-new study: Human Immunodeficiency Virus Type 1 Alters Brain-Derived Neurotrophic Factor Processing in Neurons – (07/12/12) Journal of Neuroscience paper
WASHINGTON – Researchers at Georgetown University Medical Center appear to have solved the mystery of why some patients infected with HIV, who are using antiretroviral therapy and show no signs of AIDS, develop serious depression as well as profound problems with memory, learning, and motor function. The finding might also provide a way to test people with HIV to determine their risk for developing dementia.
They say the answer, published in the July 11 issue of the Journal of Neuroscience, may ultimately lead to a therapeutic solution that helps these patients as well as others suffering from brain ailments that appear to develop through the same pathway, including those that occur in the aged.
“We believe we have discovered a general mechanism of neuronal decline that even explains what happens in some elderly folks,” says the study’s lead investigator, Italo Mocchetti, Ph.D., professor and vice chair of the department of neuroscience at Georgetown University Medical Center. “The HIV-infected patients who develop this syndrome are usually quite young, but their brains act old.”
The research team found that even though HIV does not infect neurons, it tries to stop the brain from producing a protein growth factor – mature brain derived neurotrophic factor (mature BDNF) – that Mocchetti says acts like “food” for brain neurons. Reduced mature BDNF results in the shortening of the axons and their branches that neurons use to connect to each other, and when they lose this communication, the neurons die.
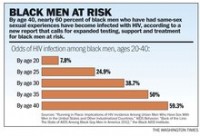
“The loss of neurons and their connections is profound in these patients,” Mocchetti says. HIV-associated dementia occurs in two to three percent of HIV-infected patients using retroviral therapies, all of who appear to be otherwise healthy, and in 30 percent of HIV-positive patients who are not on medication.
Mocchetti believes that HIV stops production of mature BDNF because that protein interferes with the ability of the virus to attack other brain cells. It does this through the potent gp120 envelope protein that sticks out from the viral shell – the same protein that hooks on to brain macrophages and microglial cells to infect them. “In earlier experiments, when we dumped gp120 into neuronal tissue culture, there was a 30-40 percent loss of neurons overnight. That makes gp120 a remarkable neurotoxin.”
This study is the product of years of work that has resulted in a string of publications. It began when Mocchetti and his colleagues were given a grant from the National Institutes on Drug Abuse to determine whether there was a connection between the use of cocaine and morphine, and dementia. (A substantial number of HIV-positive patients have been or currently are intravenous drugs users.)
They found that it was the virus that was responsible for the dementia, not the drugs, and so they set out to discover how the virus was altering neuronal function.
Their scientific break came when the researchers were able to study the blood of 130 women who were enrolled in the 17 year-old, nationwide WIHS (Women’s Interagency HIV Study, directed at Georgetown by Mary Young, M.D.), which has focused on the effects of HIV in infected females. In one seminal discovery, Mocchetti and colleagues found that when there was less BDNF in the blood, patients were at risk of developing brain abnormalities. He published this finding in 2011 in the May 15 issue of AIDS (below).
In this study, Mocchetti, Alessia Bachis, Ph.D., and their colleagues studied the brains of HIV-positive patients who had died, and who had developed HIV-associated dementia. They also found that neurons had shrunk, and that mature BDNF had substantially decreased.
He and his colleagues then worked out the mechanism responsible for this destruction of neurons.
Normally, neurons release a long form of BDNF known as proBDNF, and then certain enzymes, including one called furin, cleave proBDNF to produce mature BDNF, which then nurtures brain neurons. When uncut, proBDNF is toxic, leading to “synaptic simplification”, or the shortening of axons. It does this by binding to a receptor, p75NTR, that contains a death domain.
“HIV interferes with that normal process of cleaving proBDNF, resulting in neurons primarily secreting a toxic form of BDNF,” Mocchetti says. The same imbalance between mature BDNF and proBDNF occurs as we age, he says, although no one knows how that happens. “The link between depression and lack of mature BDNF is also known, as is the link to issues of learning and memory. That’s why I say HIV-associated dementia resembles the aging brain.”
Loss of mature BDNF has also been suggested to be a risk factor in chronic diseases such as Parkinson’s and Huntington’s diseases, Mocchetti says.
The findings suggest a possible therapeutic intervention, he adds. “One way would be to use a small molecule to block the p75NTR receptor that proBDNF uses to kill neurons. A small molecule like that could get through the blood-brain barrier.
“If this works in HIV-dementia, it may also work in other brain issues caused by proBDNF, such as aging,” Mocchetti adds.
The finding also suggests that measuring proBDNF in HIV-positive patients may provide a biomarker of risk for development of dementia, he adds.
“This finding is extremely important for both basic scientists and physicians, because it suggests a new avenue to understand, and treat, a fairly widespread cause of dementia,” Mocchetti says.
—————–
AIDS: 15 May 2011
HIV-1 decreases the levels of neurotrophins in human lymphocytes: “Serum levels of brain-derived neurotrophic factor (BDNF) were measured by an enzyme-linked immunosorbent assay in human samples collected between 1994 and 2007 at the Washington, District of Columbia site of the Women’s Interagency HIV Study…….Our main finding is that the serum of HIV-positive women is characterized by reduced levels of BDNF……This was confirmed by direct evidence that both R5 and X4 HIV-1 strains downregulate BDNF mRNA levels in T cells……recent data have shown a relationship between BDNF in blood and Alzheimer’s disease [20] and age-related cognitive impairment…….serum BDNF could be a predictor of risk for the development of neurological signs in HIV-positive individuals…….Our findings of an association between HIV infection and serum BDNF levels, and of lowered BDNF mRNA levels in infected T cells, provide initial evidence in support of this hypothesis and suggest this neurotrophin as a possible biomarker for HIV dementia. Additional studies are needed to validate our results and extend them to both sexes, as we examined a relatively small cohort of women individuals. Also, a link between BDNF and cognitive performance needs to be established.”
aDepartment of Neuroscience, Georgetown University Medical Center, Washington, District of Columbia, USA bDepartment of Microbiology and Immunology, Institute of Human Virology, University of Maryland, Baltimore, USA cLaboratory of Molecular Medicine and Neuroscience, National Institute of Neurological Disorders and Stroke/National Institute of Health, Bethesda, Maryland, USA dDepartments of Psychiatry and Psychology, University of Illinois at Chicago, Chicago, Illinois, USA eDepartment of Neurology, USA fDepartment of Medicine, Georgetown University Medical Center, Washington, District of Columbia, USA.
Abstract
Neurotrophins control cell survival. Therefore, we examined whether HIV-1 reduces neurotrophin levels. Serum of HIV-positive individuals exhibited lower concentrations of brain-derived neurotrophic factor (BDNF), but not of other neurotrophins, than HIV-negative individuals. In addition, R5 and X4 strains of HIV-1 decreased BDNF expression in T cells. Our results support the hypothesis that reduced levels of BDNF may be a ris
Neurotrophins [1,2] are produced by immune organs and immunocompetent cells, including T cells [3] and macrophages [4], and are believed to play a role in various functions of the immune system, including lymphocyte proliferation [5,6]. Little is known about the effect of HIV-1 on neurotrophin levels. Loss of neurotrophin expression may impair the immune system and promote AIDS. In this study, we investigated whether HIV-1 reduces serum concentration of the neurotrophins and sought to establish a correlation between HIV infection and neurotrophin expression in T cells.
Serum levels of brain-derived neurotrophic factor (BDNF) were measured by an enzyme-linked immunosorbent assay in human samples collected between 1994 and 2007 at the Washington, District of Columbia site of the Women’s Interagency HIV Study [7,8]. Because approximately 50% of these individuals were polydrug abusers, mainly cocaine, methamphetamine and heroin, a two-way analysis of variance (ANOVA) was used to examine a potential interaction between HIV-1 and drug use and to examine each factor independently. HIV-positive individuals exhibited significantly lower levels of BDNF compared with HIV-negative controls (Fig. 1a). Drug use significantly affected BDNF levels such that the amount of BDNF in the serum of HIV-positive drug users were higher than in HIV-positive nondrug users (Fig. 1a), suggesting that polydrug use may affect serum BDNF levels in HIV-1-positive individuals. There was no interaction between drug use and serostatus on BDNF levels (P > 0.33).
Drugs of abuse [9] or HIV-1 may influence the expression of other neurotrophins. To test this hypothesis, we measured nerve growth factor (NGF) and neurotrophin-3 (NT-3) levels in the same samples. The two-way ANOVAs analyzing associations of HIV status and drug use on NGF (P = 0.516) and NT-3 (P = 0.382) were not statistically significant, and no evidence of interaction between HIV and drug use was observed for either outcome. Although we found a tendency toward lower average NGF levels in the serum of HIV-positive individuals compared with controls, the effect was not significant (P = 0.89) nor did polydrug use affect NGF levels (data not shown). Results for NT-3 levels were similarly not statistically significant (data not shown).
The reduction of BDNF observed in HIV-1-positive individuals could be due to single nucleotide polymorphisms (SNPs) that alter intracellular packaging and secretion of BDNF [10]. rs6265 is a polymorphism in the BDNF gene that produces an amino acid substitution of valine to methionine in codon 66 (Val66Met); rs56164415 is located in the fifth of the seven noncoding exons of the BDNF gene [11] and appears to be moderately associated with substance abuse [12]. Therefore, these SNPs, either alone or in combination, might lead to a reduction in serum BDNF levels. To test this hypothesis, we examined the frequency of these polymorphisms in the same cohort, using DNA from the same sample of individuals. There was no significant difference in frequency of alleles in HIV individuals as compared with HIV-negative controls (rs6265, P = 0.83; rs56164415, P = 0.72). Therefore, mutation of the BDNF gene does not appear to account for difference in the levels of BDNF in these individuals.
Contributing factors that may account for the decrease in serum BDNF in HIV-positive individuals are not easily defined. BDNF and other neurotrophins are produced by immune organs and immunocompetent cells [13], as well as platelets [14]. Thus, a decrease in the number of platelets may explain the lower levels of BDNF in HIV-1-positive individuals. To determine whether BDNF from platelets constitutes a significant fraction of serum BDNF, we examined which blood cell type expresses BDNF. We found that platelets and T cells exhibited comparable levels of BDNF expression (Fig. 1b). Thus, platelets account for only for a fraction of serum BDNF. Nevertheless, to more directly examine the effect of HIV-1 on BDNF, we examined the ability of HIV-1 to decrease BDNF expression in T cells. T lymphocytes were prepared from healthy donors and were infected with X4 (IIIB) or R5 (BaL) HIVs. BDNF mRNA levels were then quantified 24 h after the infection. We observed an approximately 50% decrease in BDNF mRNA levels by both HIV-1 strains (Fig. 1c), further suggesting that HIV-1 is capable of reducing the expression of this neurotrophin in T cells.
Our main finding is that the serum of HIV-positive women is characterized by reduced levels of BDNF, but not of NGF or NT-3, irrespective of drug use status, suggesting that HIV-1 influences the expression of selected neurotrophins. This was confirmed by direct evidence that both R5 and X4 HIV-1 strains downregulate BDNF mRNA levels in T cells. These results may contribute new insights into our understanding of the immune dysregulation of AIDS. In fact, given the well known antiapoptotic effect of the neurotrophins for T cells [6,13], we may speculate that a decrease in BDNF could be among the mechanisms employed by HIV-1 to induce apoptosis of T cells. On the contrary, experimental evidence has shown an inverse correlation between levels of BDNF and CXCR4 [15] and CCR5 [16] expression. These coreceptors are crucial for HIV-1 infection [17]. Therefore, reduced levels of BDNF may be a risk factor for increasing HIV infection.
HIV-1 also causes axonal injury, neuronal loss and dementia [18]. BDNF is critical for neuronal survival [19]. Blood neurotrophin levels have been used to investigate the role of the neurotrophins in the pathogenesis of various neurodegenerative diseases. In fact, recent data have shown a relationship between BDNF in blood and Alzheimer’s disease [20] and age-related cognitive impairment [21]. Therefore, serum BDNF could be a predictor of risk for the development of neurological signs in HIV-positive individuals. Our findings of an association between HIV infection and serum BDNF levels, and of lowered BDNF mRNA levels in infected T cells, provide initial evidence in support of this hypothesis and suggest this neurotrophin as a possible biomarker for HIV dementia. Additional studies are needed to validate our results and extend them to both sexes, as we examined a relatively small cohort of women individuals. Also, a link between BDNF and cognitive performance needs to be established. |
 A demonstrator holds up paper dolls, which were usedas message boards for people to write their thoughts on female condoms during the 19th International AIDS Conference in Washington, DC on July 24.
A demonstrator holds up paper dolls, which were usedas message boards for people to write their thoughts on female condoms during the 19th International AIDS Conference in Washington, DC on July 24.




 e trial known as HVTN505. This trial is currently enrolling 2,200 men who have sex with men (MSM) in the US who are circumcised and who have not been previously exposed to a common cold virus known as adenovirus serotype 5 (Ad5), a modified version of which is being used as the vector that delivers the active ingredients of the vaccine under evaluation (see VAX Sep. 2011
e trial known as HVTN505. This trial is currently enrolling 2,200 men who have sex with men (MSM) in the US who are circumcised and who have not been previously exposed to a common cold virus known as adenovirus serotype 5 (Ad5), a modified version of which is being used as the vector that delivers the active ingredients of the vaccine under evaluation (see VAX Sep. 2011