On this annual day of remembrance, we pause to reflect on the state of science, policy, activism, treatment, and prevention and to renew energy and partnerships in our shared goal of ending HIV/AIDS.
We celebrate that improvements in HIV medications have made it so that people living with HIV can remain virally suppressed for long stretches of time – and that the life expectancy of those who are HIV-infected and on treatment is the same as those who are not HIV-infected. Treatment improves and maintains the health of those living with HIV and prevents transmission of HIV to others.
Treatment as Prevention (TasP) works! Undetectable=Untransmittable (U=U).
We celebrate that we have powerful new tools to add to the existing HIV prevention armamentarium. The use of an HIV medication can prevent transmission among people who are at high risk for HIV exposure, especially when the HIV medication is combined with behavioral prevention.
Pre-Exposure Prophylaxis (PrEP) works!
We celebrate that there is promise in the medication development pipeline! Not long from now, use of long-acting formulations of HIV medications will make it so that people living with HIV no longer need to take pills daily to maintain viral suppression. These long-acting HIV medications are likely to provide coverage for prevention, too—though that’s further in the future. New approaches, like using monoclonal antibodies, are under development and hold promise for treatment and prevention.
Never before has there been so many effective medications that can be combined with behavioral strategies for HIV treatment and prevention. Yet, this progress has not benefited all individuals who are living with or are at-risk for HIV/AIDS equally. Today, substantial numbers of people are living with HIV and are not virally suppressed. Too many people who are at risk for HIV cannot, will not, or do not take advantage of our powerful toolbox of HIV prevention methods.
For this reason, we propose a call, as a community, to renew policy and energy to address HIV treatment and prevention, in the U.S. and globally:
Let’s recognize a key truth that while most people can reach and sustain HIV treatment and prevention goals, there is a sizeable minority who cannot meet these goals with consistency.
Let’s recognize that there are real life reasons that interfere with people not being able to regularly meet their HIV treatment and prevention goals. These include chronic and disorganizing influences caused by co-occurring mental health and or substance use disorders, by stigma in all its forms, and by inconsistent access to food, housing, medical care, and other structural determinants of health.
Let’s recognize that scientific and programmatic efforts for those who cannot consistently achieve and sustain HIV treatment and prevention goals will be different (and more intensive) from that which works for the larger group who can. These efforts will likely need to include multiple disciplines and to be available when needed over the lifetime—not just one time.
Let’s use data better to figure out how best to allocate resources that meet the conditions faced both by the larger and by the smaller parts of our population who are living with or who are at risk for HIV.
Let’s build respect into the essence of this renewed direction. We do that by confronting head-on poverty, racism, sexism, homophobia, HIV stigma, homelessness at every level in our joint commitment to provide tangible packages of services that are accessible and acceptable to each and every one of us. This is foundational to a shared future with no more HIV infections.
We hope that on this World AIDS Day 2017 we can collectively harness our insights and energies to pursue these important new directions in science and programs that will get us to zero new HIV infections within the next decade. Let us all feel renewed and recharged as we move forward together with commonality of purpose and mission.


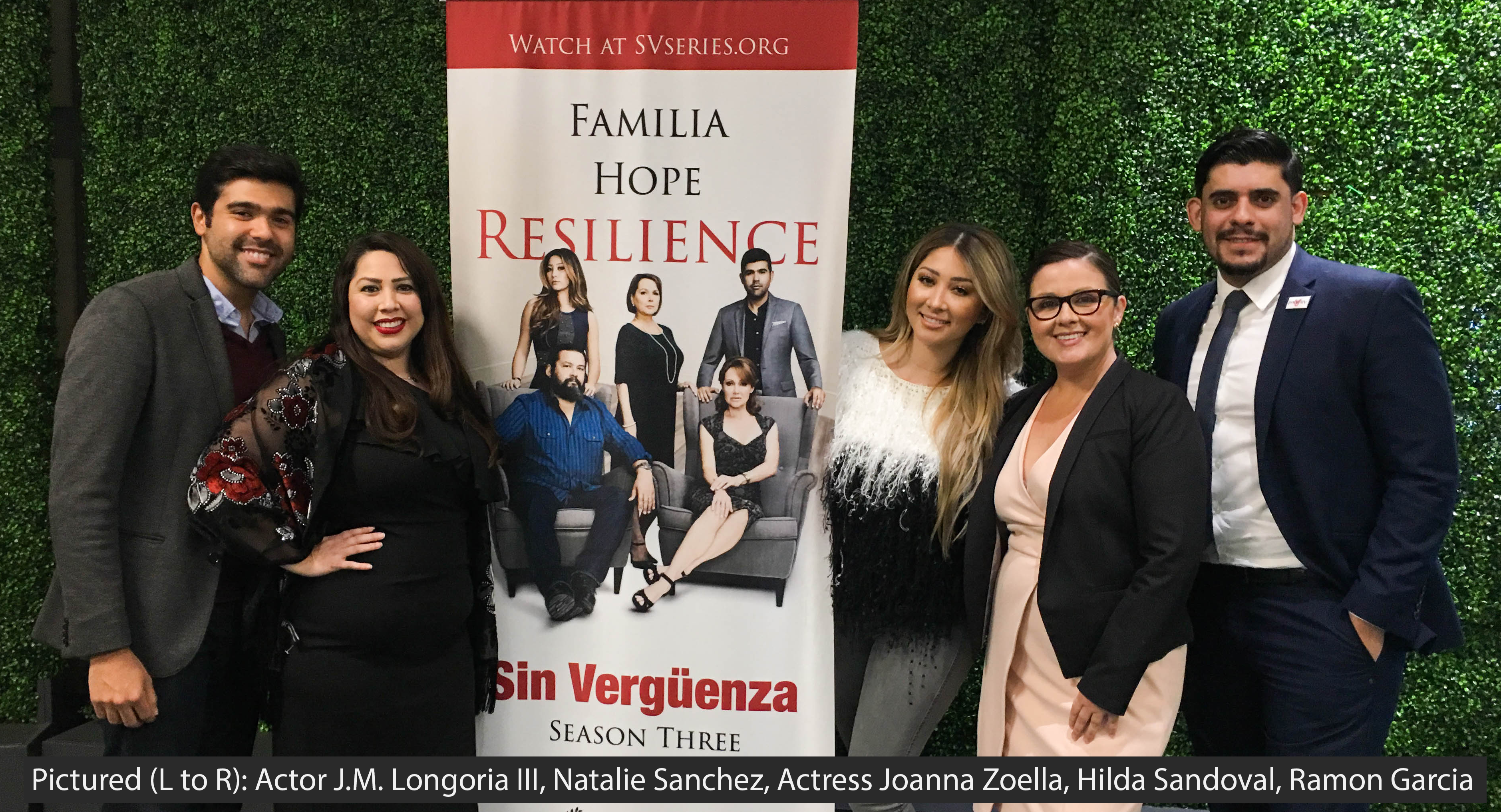

 Natalie Sanchez and Hilda Sandoval from AltaMed discussed the process of developing an HIV social marketing campaign that is relevant and accessible to Latinos across multiple generations. They also addressed how the telenovela can be a channel to address the social determinants which are identified in the Los Angeles County HIV/AIDS Strategy 2020 and Beyond. Ramon Garcia also spoke on the social impact of the series, breaking down the metrics and the reach of the videos and their goals with this new season. With the success of season’s one and two, Sanchez talked more about the use of entertaining content to increase awareness on HIV-related issues such as the ones they focused on in Season 3.
Natalie Sanchez and Hilda Sandoval from AltaMed discussed the process of developing an HIV social marketing campaign that is relevant and accessible to Latinos across multiple generations. They also addressed how the telenovela can be a channel to address the social determinants which are identified in the Los Angeles County HIV/AIDS Strategy 2020 and Beyond. Ramon Garcia also spoke on the social impact of the series, breaking down the metrics and the reach of the videos and their goals with this new season. With the success of season’s one and two, Sanchez talked more about the use of entertaining content to increase awareness on HIV-related issues such as the ones they focused on in Season 3.

 Dr. Dvora Joseph Davey came to UCLA to present on her work in South Africa in a special guest lecture titled “Evaluating Sex Behaviors and Substance Use in Pregnant Women in South Africa: Informing Interventions to Prevent HIV Acquisition and Transmission.” With over 30 attendees in the audience ranging from well-versed researchers and faculty to postdoctoral students to undergraduate students, Dr. Joseph Davey gave a thorough overview of not only the current state of HIV risk and transmission in South Africa but also the studies that are currently in place, working to understand the institutions that affect these factors and aiming to find more effective ways to prevent transmission.
Dr. Dvora Joseph Davey came to UCLA to present on her work in South Africa in a special guest lecture titled “Evaluating Sex Behaviors and Substance Use in Pregnant Women in South Africa: Informing Interventions to Prevent HIV Acquisition and Transmission.” With over 30 attendees in the audience ranging from well-versed researchers and faculty to postdoctoral students to undergraduate students, Dr. Joseph Davey gave a thorough overview of not only the current state of HIV risk and transmission in South Africa but also the studies that are currently in place, working to understand the institutions that affect these factors and aiming to find more effective ways to prevent transmission.